Injured persons are an integral part of every Out Patient Department (OPD) in a hospital. At our hospital we get around 5 to 10 injury cases every day. And there is only one thing common in all these cases… all of them want Injection TT (Tetanus Toxoid). If it is a child who gets injured, the parents drag them to the hospital just to prick them with the syringe loaded with the magical ‘TT’. I am talking about the people in my area who resist the idea of immunization of small kids. They blatantly refuse to give the small babies injections, but they want everybody to get the ‘TT’ which they consider as a medicine for wound healing, and not as a vaccine. According to these demanding patients, one dose of TT is effective only for 6 months. I have no idea where they get such ideas from and so in this post I will be dealing with the Prevention of Tetanus and some of the important misconceptions regarding the Tetanus Immunization.
Before you go into the details of Tetanus, you might want to take a look at the Universal Immunization Programme (UIP).
What is Tetanus?
Tetanus is a disease induced by the toxins (proteins) of a bacterium called the Clostridium Tetani. Clinically the symptoms mostly includes persistent muscular rigidity punctuated with spasms of voluntary muscles like the facial muscles, muscles of the back and neck. It is a dangerous disease with a high mortality rate.
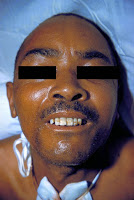 |
| Lock-Jaw Courtesy – CDC, Wikimedia Commons |
The Tetanus bacilli are spore bearing anaerobic organism adopting the shape of a ‘drumstick’. The spores germinate under anaerobic conditions (lack of air) and produces certain proteins called the ‘exotoxin’. The main reservoir of the bacilli is soil and dust. They are also found in our intestines, without causing any diseases. Tetanus occurs when the spores of the bacilli enter our body through the injured area. The range of injuries through which infection can occur are – a small pin prick, abrasion, puncture wounds, human/animal bites, stings, burns, unsterile surgery etc. They multiply in the anaerobic conditions in the wound and produces the toxins. These harmful proteins acts on our ‘central nervous system’.
We often get muscle spasms when we adopt an uncomfortable posture. Imagine such a spasm of your jaw and neck muscles which keeps on going for many days. That is why the condition is also called “Lock-Jaw”. Death finally occurs when the toxins effects the muscles of respiration (breathing). This disease is not transmitted from person to person.
Treatment of Tetanus has to be done at the hospital. The wound site is cleaned, drained (if required), proper antibiotics are given. The patient is monitored for any signs of respiratory failure (breathing difficulties) during the course of the treatment. The main angle of treatment is to stop the toxin production, neutralize the effect of toxins and control muscle spasms. Anti-toxins are given to the patient to neutralize the effect of the toxins. Muscle relaxants are used to control the muscle spasms. In severe cases, patient might be put on artificial breathing machines.
Tetanus in India
There were about 11,000 cases of Neonatal Tetanus (neonates are babies aged less than 28 days) in India in 1989 and this has decreased to 528 cases by 2013. This has been made possible by the implementation of various programmes like giving two doses of Tetanus Toxoid to every pregnant woman, including Tetanus Toxoid in the Universal Immunizatin Programme (UIP), increasing the number of Institutional deliveries, giving proper training for health workers as part of the NRHM programme etc.
Prevention of Tetanus
First of all – make sure that the wound is cleaned thoroughly. Remove the soil, dust, foreign bodies if any, dead tissue. This will prevent the formation of anaerobic conditions which is required for the spores to germinate and multiply.
Active Immunization are of two types.
Monovalent Tetanus Toxoid – 2 doses of TT are given one month apart and a booster after one year. One more booster may be given only after 5 years of giving the first booster. Repeated booster doses are not advised and must be avoided. Active Immunization however does not confer immediate protection because an effective Immune response needs to be produced in our bodies and that takes it’s own time.
Combined vaccines – Tetanus toxoid combined with Diphtheria and Pertussis vaccines and given as DPT vaccine as part of UIP. It is given as 3 doses, 4 weeks apart starting from 6 weeks after birth and a booster is given at 18 months of age.
Passive Immunization are for immediate protection following an injury. This is achieved by giving human or equine tetanus immunoglobulins. This is entirely different from the Tetanus Toxoid mentioned earlier. These injections (anti sera) can be allergic for some persons and hence the emergency medicines should be kept ready before administering the injection.
Antibiotics should be given with the immunization to prevent other bacterial growth in the wounded area. Giving Tetanus Toxoid doesn’t protect you from getting infected immediately, and passive immunization with anti-sera has many drawbacks as mentioned earlier. This is why antibiotics are given even to prevent Tetanus. A single dose of penicillin injection will prevent active growth of the vegetative forms of the Tetanus bacilli for about 3 weeks.
Inj. Tetanus Toxoid 0.5ml IM stat
In order to make things more clear, let us classify the various types of injuries into two groups. Let group “A” denote those injuries which are clean, trivial, non penetrating and with negligible tissue loss. And let all other nasty wounds with tissue loss belong to group “B”.
Patients in group “A” who were fully immunized earlier, require one dose of Toxoid if last booster was taken 5+ years ago. If their immune status is unknown, complete course of Toxoid has to be given i.e., 2 doses one month apart and a booster after one year.
Patients in group “B” who were fully immunized earlier with history of a booster dose taken within 5 to 10 years requires one dose of Toxoid. If they have clear history of booster taken more than 10 years ago, they need Human Tetanus Immunoglobulin along with one dose of Toxoid. And lastly, if their previous immunisation history is unknown, patient needs a complete course (2+1) of Toxoid along with Human Tetanus Immunoglobulin.
*Fully Immunized persons are those who have taken 2 doses of TT one month apart and then a booster dose taken after one year of the first dose.
Final Words
Tetanus toxoid and anti sera are very effective in preventing Tetanus. Proper wound care is also necessary for prevention along with Immunization. Neonatal Tetanus is one of the major killer disease of the newborns in India and it can be prevented only by strengthening the Immunization Programmes. I hope this article will help you in deciding whether you require a TT injection or not after you injure yourselves. Tell me what you think in the comments below.
TT 🙂
You didn’t tell if complete course gives lifelong immunity
Booster doses are meant to “booost” the immunity. Lifelong immunity is thus irrelevant here.
Also this booster doses program was not prevelant probably 20 years ago, so what’s there status considered. They had only 1 or 2 dpt shots one mostly back then